GustavsonMex2.0
Oakley Beginner
- 88
- 83
Gracias amigo ! Im just waiting to get vaccinated But here in Mexico... we are the #2 on death tolls 1, 500 at day!
250,000,00 deaths.
250,000,00 deaths.
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: this_feature_currently_requires_accessing_site_using_safari


Experts like who? Fauci? None of these people know $hit about this virus. Vaccine isnt even working. double vaccinated people are still getting covid lol.Do Vaccines Reduce Transmission?
- Experts say it appears that COVID-19 vaccines can help reduce the transmission of the new coronavirus from person to person.
- They say this is accomplished by reducing the viral load in a vaccinated person’s nose.
- Experts say until further studies are done, vaccinated people should still abide by safety protocols such as mask wearing and physical distancing.

COVID-19 Vaccines May Help Stop Virus Transmission
Early evidence suggests that COVID-19 vaccines may reduce the chance that a vaccinated person will transmit the virus to others.www.healthline.com
Researchers saw an 89 percent drop in asymptomatic infections among this group compared with an unvaccinated comparison group. These results haven’t been published yet in a peer-reviewed journal.
86% drop in asymptomatic cases AFTER vaccination in Pfizer or AstraZeneca vaccines

Effectiveness of BNT162b2 mRNA Vaccine Against Infection and COVID-19 Vaccine Coverage in Healthcare Workers in England, Multicentre Prospective Cohort Study (the SIREN Study)
Background: BNT162b2 mRNA and ChAdOx1 nCOV-19 adenoviral vector vaccines have been rapidly rolled out in the UK. We determined the factors associated with vaccipapers.ssrn.com
J&J showed a 74% drop in asymptomatic cases

 www.dentistrytoday.com
www.dentistrytoday.com  journals.sagepub.com
journals.sagepub.com 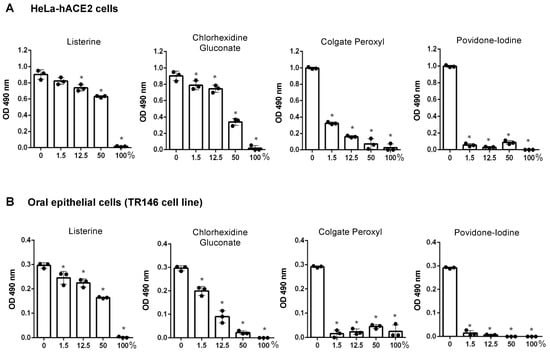
Time to inject it then .......Dental - Some Toothpastes Can Help Neutralise COVID-19
Toothpastes that include zinc or stannous and mouthwash formulas with cetylpyridinium chloride (CPC) neutralize SARS-CoV-2 by 99.9%, according to Colgate.

Some Toothpastes and Mouthwashes Neutralize the COVID-19 Virus by 99.9% - Dentistry Today
Toothpastes that include zinc or stannous and mouthwash formulas with cetylpyridinium chloride (CPC) neutralize SARS-CoV-2 by 99.9%, according to Colgate.www.dentistrytoday.com
83.6% of patients had anomalies of the oral cavity or nearby structures at approximately 3 mo after hospital discharge.
Of importance, anti-SARS-CoV-2 antibodies were found to be readily detectable in patients’ saliva for at least 3 mo after symptom onset (Isho et al. 2020; Pisanic et al. 2020), clearly pointing to the oral cavity as a privileged immune site during COVID-19.
SAGE Journals: Your gateway to world-class research journals
Subscription and open access journals from SAGE Publishing, the world's leading independent academic publisher.journals.sagepub.com
2 types of mouthwashes may have the potential to disrupt the COVID-19 virus from replicating in human cells. Listerine and the prescription mouthwash Chlorhexidine, were able to disrupt the virus within just seconds. Additionally, 2 other types of mouthwash showed promise for potentially providing protection in preventing viral transmission. These 2 were Betadine, which contains povidone iodine, and Peroxal, which contains hydrogen peroxide.
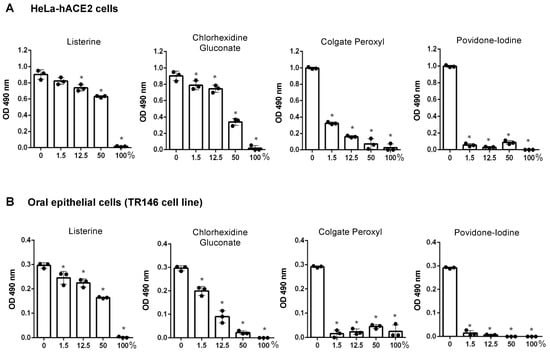
Differential Effects of Antiseptic Mouth Rinses on SARS-CoV-2 Infectivity In Vitro
Severe acute respiratory syndrome-related coronavirus (SARS-CoV-2) is detectable in saliva from asymptomatic individuals, suggesting a potential benefit from the use of mouth rinses to suppress viral load and reduce virus spread. Published studies on the reduction of SARS-CoV-2-induced cytotoxic...www.mdpi.com
Both the Pfizer and Moderna vaccines had effective rates of over 95% in clinical trials. Notice how that number isn’t 100%?Experts like who? Fauci? None of these people know $hit about this virus. Vaccine isnt even working. double vaccinated people are still getting covid lol.
"Experts"
Totally agreeBoth the Pfizer and Moderna vaccines had effective rates of over 95% in clinical trials. Notice how that number isn’t 100%?
Even more effective at reducing severe illness and hospitalisation. The flu vaccine is typically somewhere around 60% effective in any given year and yet still brings the death rate down. The Covid vaccines are much more effective than that.
Zero Covid isn’t the goal, certainly not foe now. Minimising death and severe illness is.
Both the Pfizer and Moderna vaccines had effective rates of over 95% in clinical trials. Notice how that number isn’t 100%?
Even more effective at reducing severe illness and hospitalisation. The flu vaccine is typically somewhere around 60% effective in any given year and yet still brings the death rate down. The Covid vaccines are much more effective than that.
Zero Covid isn’t the goal, certainly not for now. Minimising death and severe illness is.

