Variants

CDC, WHO Establish New Threat Levels for COVID-19 Variants
New designation levels will help clarify what's known about circulating viruses, and then help explain risk.
www.medscape.com
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: this_feature_currently_requires_accessing_site_using_safari

 www.who.int
www.who.int Yep, we’ll be in a cycle of annual boosters, amended for new circulating variants.Covid will always be around now, just like the flu
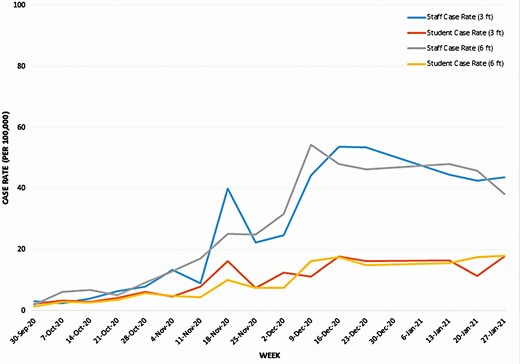
 science.sciencemag.org
science.sciencemag.org 

Individual | Risk factors | “Covid-age” | Estimated mortality if infected (range of uncertainty) |
|---|---|---|---|
Your patient | 60 year old woman White BMI <30 Type 2 diabetes Rheumatoid arthritis | 71 | 14 per 1000 (7 to 28 per 1000); ~1 in 70 chance of dying |
Your patient without medical risk factors | 60 year old female White BMI <30 | 55 | 3 per 1000 (1 to 5 per 1000); ~1 in 333 chance of dying |
High risk friend (father of groom) | 75 year old man Asian BMI 35-39.9 Heart failure | ≥85 | 60 per 1000 (30 to 119 per 1000); ~1 in 8 chance of dying |
Low risk friend (daughter) | 31 year old woman White BMI <30 | 26 | 0.1 per 1000 (0.07 to 0.3 per 1000); ~1 in 10 000 chance of dying |